By Sheryl Gay Stolberg, The New York Times
President Joe Biden, confronting a worrisome new coronavirus variant and the potential of a winter surge, laid out a new pandemic strategy on Thursday afternoon that includes hundreds of vaccination sites aimed at families, booster shots for all adults, new testing requirements for international travelers and insurance reimbursement for at-home coronavirus tests.
The push to expand access to at-home testing is a tacit acknowledgment by the White House that vaccination, which the president has touted as the path out of the pandemic, is not enough on its own. Experts have argued for months that mask-wearing and testing are also essential, and the need for testing will become even more urgent if the Omicron variant is found to evade protection from vaccines, which has not yet been established.
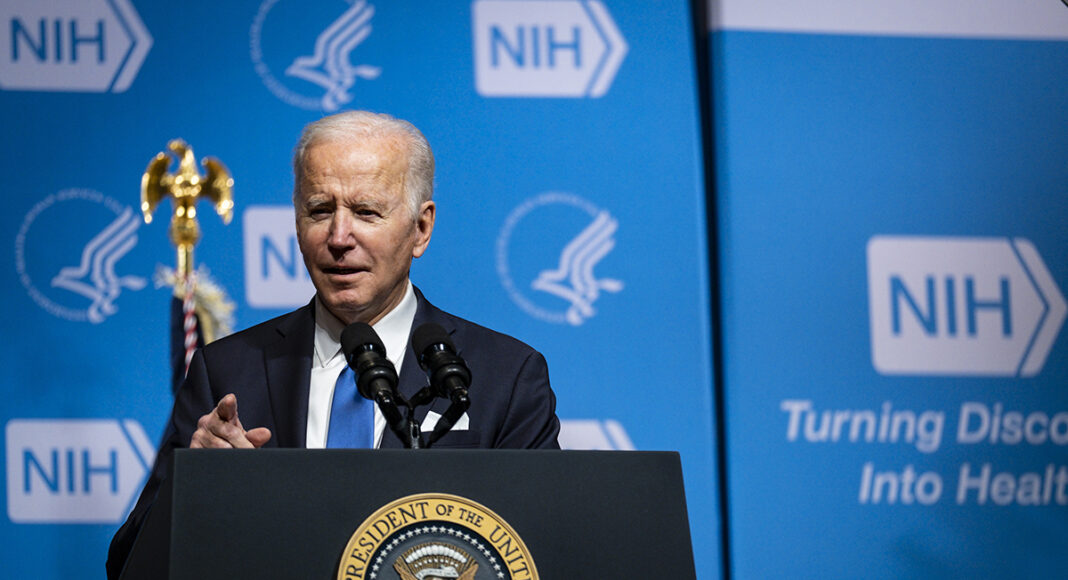
“We’re going to fight this variant with science and speed, not chaos and confusion,” the president said at the National Institutes of Health.
Biden’s announcement comes a day after the new Omicron variant was detected in the United States for the first time, in California. On Thursday, a second case was detected, in a Minnesota resident who had recently traveled to New York City. Experts said the announcement on testing was particularly important.
“We agree with an applaud the fact that the president is taking a holistic view,” Dr. Nirav Shah, president of the Association of State and Territorial Health Officials, adding, “for this next phase of the pandemic, rapid access to rapid testing will be key.”
Senior administration officials, speaking on condition of anonymity to preview the plan Thursday night, said it was aimed at keeping the economy, workplaces and schools open.
A big part of the plan is a renewed push to get people vaccinated, including the latest group to become eligible, children ages 5 to 11. The administration plans to launch “hundreds of family vaccination clinics” that will offer vaccinations and boosters for people of all eligible ages, according to a fact sheet provided by the White House.
The plan also includes a national campaign to reach the 100 million Americans who are eligible for booster shots and have not had them. The campaign will include paid advertising and free rides to vaccination sites coordinated by AARP, the advocacy group for older Americans. And the Federal Emergency Management Agency will launch what the administration is calling Family Mobile Vaccination Clinics, beginning with deployments to Washington and New Mexico. The goal is for states and localities to replicate the model “with full federal funding and support,” officials said.
Biden called on employers to provide paid time off for employees to get boosters.
Biden’s new strategy will extend the current mask mandate for people on airplanes, trains and buses, and in terminals and transit hubs, through mid-March. But the president, who put a strong emphasis on mask-wearing at the outset of the pandemic, does not appear poised to call on governors to revive the mask mandates that many of them abandoned.
Only six states now require people to wear masks in indoor public settings regardless of their vaccination status. Three more — California, New York and Connecticut — require masks indoors for people who are unvaccinated.
Biden ran for office in 2020 on a promise to get the pandemic under control. Since then, though, the virus “has thrown us a number of curveballs, and unfortunately they were thrown at 200 miles an hour,” said Michael T. Osterholm, who directs the Center for Infectious Disease Research and Policy at the University of Minnesota.
Many experts predict a surge in the United States over the winter, regardless of whether the Omicron variant spreads widely in the country. The nation has been reporting an average of more than 80,000 new cases a day over the last few weeks, according to a New York Times database; six months ago, the average was roughly 12,000 new cases a day.
Much remains unknown about the Omicron variant, which was first spotted by scientists in southern Africa and now known to be present in more than 30 countries including the United States. It has mutations that scientists say may allow it to spread more quickly and cause more breakthrough infections in vaccinated or previously infected people, though neither characteristic has yet been confirmed.
Under the president’s plan, at-home tests would be reimbursed for the 150 million Americans with private insurance. To ensure access for those who lack insurance, or who are covered by Medicaid, the administration intends to distribute an additional 15 million tests to community health centers and rural clinics.
Looking forward, experts envision a world where people will test themselves as soon as they exhibit symptoms — and then, if they are positive, would go into quarantine and seek treatment with new antiviral medicines that are in development. Early testing is important because the antivirals work best just after the onset of symptoms. The White House says it is taking steps to secure 13 million courses of antiviral treatments.
In the United States, home coronavirus tests have been relatively hard to come by because of supply shortages, and they are expensive — as much as $25 apiece. Dr. Carlos del Rio, an infectious disease specialist at Emory University, said that rather than have people go through the cumbersome process of seeking insurance reimbursement for tests, “we should just subsidize them and make it incredibly cheap.”
In Britain, he noted, rapid tests are free, and in Germany they cost consumers about $1 apiece.
Reimbursement for at-home tests in the United States will not happen immediately, and will not be retroactive, the senior administration officials said, adding that federal agencies would issue guidance by Jan. 15 to clarify that insurers would have to reimburse people for at-home tests during the COVID-19 public health emergency.
It was unclear how many tests a person could be reimbursed for buying, or how the reimbursement would work. Shah, of the state health officials association, said his group would prefer that people get reimbursed when they buy the tests in pharmacies, as opposed to having to file later for reimbursement.
Private insurers already cover the cost of coronavirus tests administered in doctor’s offices and other medical facilities. At least eight at-home tests are on the U.S. market.
This article originally appeared in The New York Times.